What is diabetes-related retinopathy?
Diabetes damages blood vessels throughout the body, because increased sugar levels are harmful to blood vessels.
The retina, which is responsible for detecting light and sending messages to the brain to form pictures, is very delicate and is covered in blood vessels. Damaged blood vessels in the retina is known as diabetes-related retinopathy and arises due to leakage and blockage of blood vessels.
Stages
Diabetes-related retinopathy is classified into 4 main stages, which helps doctors categorise how to monitor and treat patients.
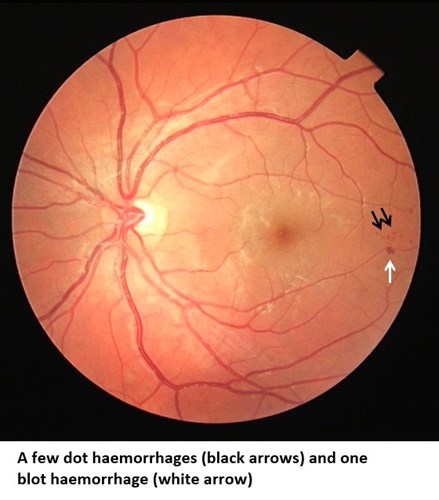
Background diabetes-related retinopathy (R1):
This is a very early stage of retinopathy that is low risk and requires no treatment. People with these changes are screened annually with a photo. Improved blood sugar and blood pressure control are advised as this reduces the chance of worsening eye changes.
Pre-proliferative retinopathy (R2):
In this stage, the background retinopathy has progressed and is much more extensive. The retina can become starved of oxygen, called ischaemia, which increases the risk of sight loss. Close monitoring in the hospital eye service is needed; further investigations and specific treatments may also be required.

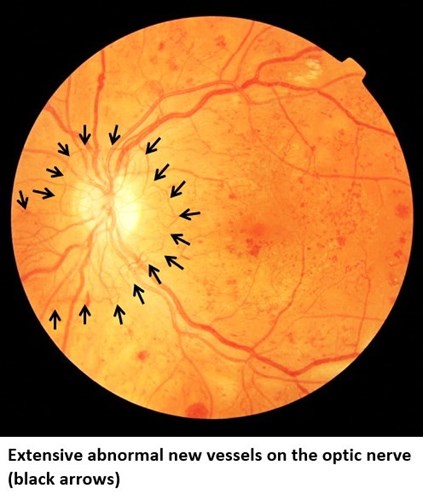
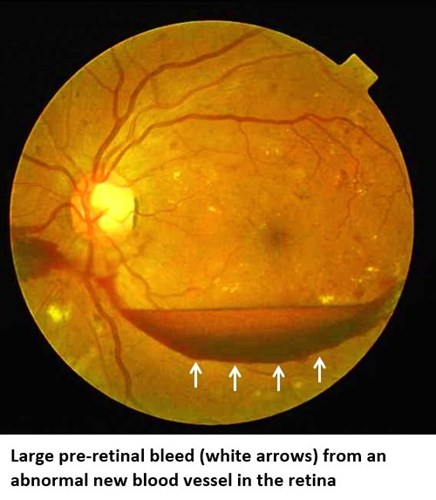
Proliferative retinopathy (R3A):
As the oxygen level in the retina decreases, new abnormal blood vessels start to grow. These new vessels are very fragile, and can lead to large bleeds, scarring or the retina can pull off. This is a very serious stage of eye disease that needs urgent treatment and can lead to permanent blindness if not treated.
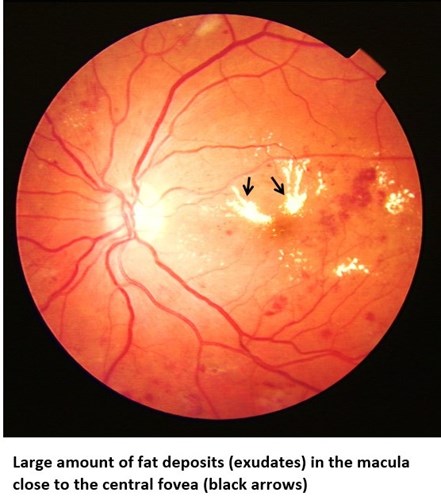
Maculopathy (M1):
The macula is the central part of the retina that is responsible for fine detailed vision. Small changes in the macula, such as those seen in background retinopathy, are known as maculopathy. These can develop together with any of the stages of retinopathy described above. This needs close monitoring in the hospital eye service and may require treatment.
Further resources
Find out more about maculopathy on the Macular Society website




